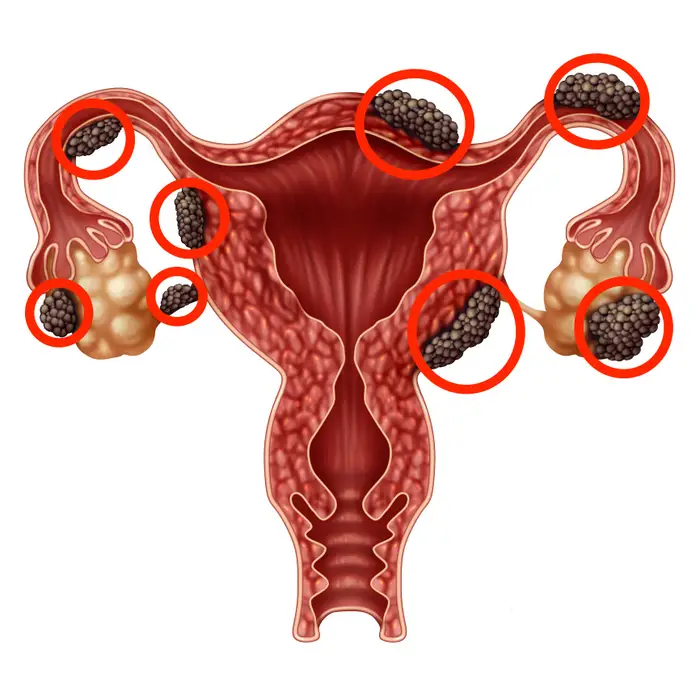
Endometriosis is a chronic and often painful gynecological condition that affects about 10% of women of reproductive age worldwide. It occurs when the tissue that normally lines the uterus (called the endometrium) grows outside of the uterus, most commonly on the ovaries, fallopian tubes, and tissue lining the pelvis.
The exact cause of endometriosis is unknown, but there are several theories.
The oldest of these theories is one called retrograde flow, however this theory is now thought to be incorrect. The retrograde flow theory suggests that during menstruation, some of the endometrial tissue flows backwards through the fallopian tubes and into the pelvic cavity, where it can implant and grow.
More up-to-date theories suggest that endometrial cells may be present in the pelvis from birth, or that the immune system may play a role in the development of endometriosis.
Endometriosis can cause a range of symptoms, including chronic pelvic pain, painful periods, pain during or after sexual intercourse, and infertility. These symptoms can have a significant impact on a woman’s quality of life.
Diagnosis of endometriosis can be difficult, as the symptoms often overlap with those of other conditions, such as ovarian cysts or pelvic inflammatory disease. A combination of pelvic exam, imaging tests, and laparoscopic surgery (a surgical procedure in which a small camera is inserted through a small incision in the abdomen) is often used to diagnose endometriosis.
Treatment for endometriosis typically involves a combination of medications and surgery. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, can help to reduce pain. Hormonal therapies, such as birth control pills, can help to regulate the menstrual cycle and reduce the growth of endometrial tissue. In more severe cases, surgery may be necessary to remove the endometrial tissue.
There is no cure for endometriosis, and the condition can recur after treatment. Researchers are continuing to study the condition in order to better understand its causes and to develop more effective treatments.
One area of focus is the role of inflammation in the development and progression of endometriosis. Inflammation is the body’s natural response to tissue damage or infection, and it is thought to play a role in the growth of endometrial tissue outside of the uterus. Some studies have suggested that anti-inflammatory drugs may be effective in the treatment of endometriosis, although more research is needed to confirm this. In our clinical experience, the use of the Flourish Anti-inflammatory blend assists in this.
Another area of research is the use of stem cells in the treatment of endometriosis. Stem cells are unspecialized cells that have the ability to develop into different types of cells, and they have shown promise in the treatment of a number of conditions. Some studies have suggested that stem cells may be able to regenerate damaged tissue and reduce inflammation, making them a potential treatment option for endometriosis.
Other researchers are looking at the role of genetics in the development of endometriosis. Some studies have identified genetic variations that may be associated with an increased risk of developing the condition. Understanding the genetic basis of endometriosis may help to identify women who are at high risk for the condition, and may also lead to the development of targeted treatments.
Overall, endometriosis is a complex and poorly understood condition that can have significant impacts on a woman’s quality of life. While more research is needed to fully understand the condition and to develop more effective treatments, progress is being made, and there is hope for women who are living with endometriosis.
There is limited research on the relationship between diet and endometriosis. However, some studies have suggested that certain dietary factors may play a role in the development and progression of the condition.
One dietary factor that has been studied in relation to endometriosis is consumption of dairy products. Some research has suggested that high intake of dairy products may be associated with an increased risk of endometriosis. Other studies have found no association between dairy intake and endometriosis risk. More research is needed to determine the relationship between dairy consumption and endometriosis.
Another dietary factor that has been studied in relation to endometriosis is consumption of soy products. Some studies have suggested that high intake of soy may be associated with a reduced risk of endometriosis. Soy contains compounds called isoflavones, which have estrogen-like effects in the body and may help to regulate the menstrual cycle. However, more research is needed to confirm the relationship between soy consumption and endometriosis.
There is also some evidence to suggest that a diet high in fruits and vegetables may be beneficial for women with endometriosis. Fruits and vegetables are rich in antioxidants, which may help to reduce inflammation in the body. Some studies have found that women with endometriosis who have a high intake of fruits and vegetables have a lower risk of the condition.
It is important to note that while some dietary factors may be associated with an increased or decreased risk of endometriosis, it is not clear whether these factors cause the condition. Additionally, the relationship between diet and endometriosis is complex and may be influenced by other factors, such as genetics and lifestyle.
In general, a healthy diet that is rich in fruits and vegetables, whole grains, and plant proteins is recommended for women with endometriosis. It is also important to stay hydrated and to limit intake of processed and high-fat foods.
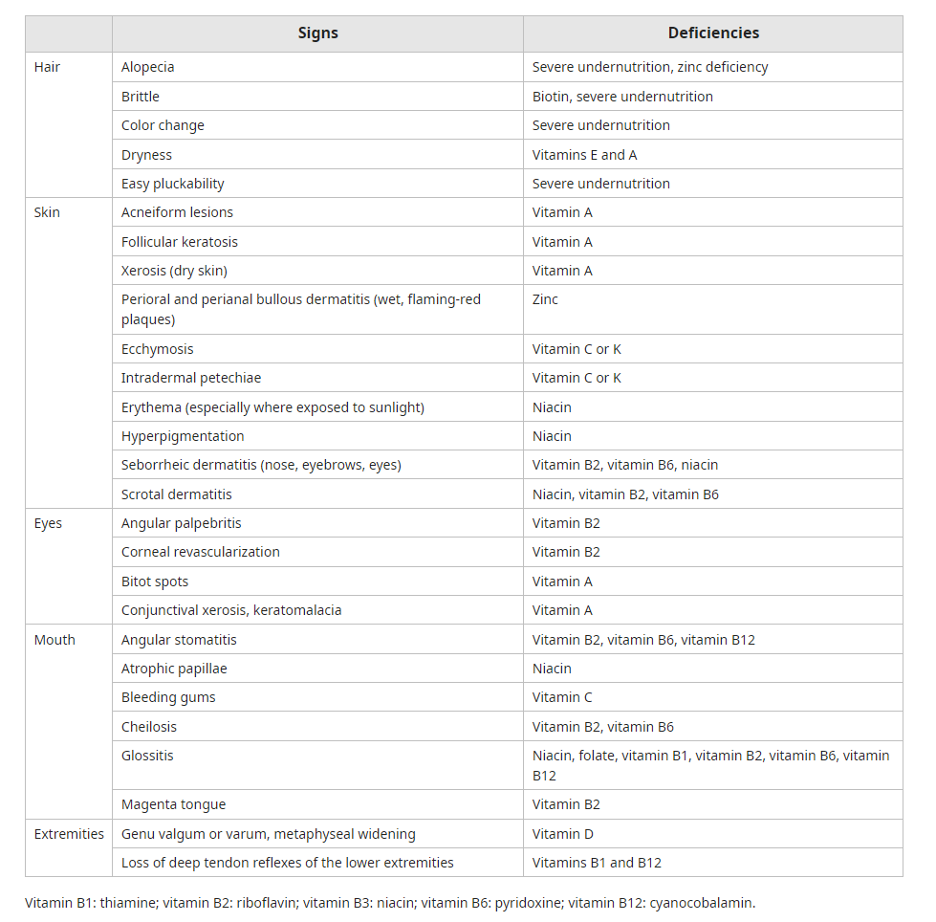
There is also some evidence to suggest that certain nutrient deficiencies may be associated with an increased risk of endometriosis. However, it is not clear whether these nutrient deficiencies cause the condition or if they are a result of the condition.
One nutrient that has been studied in relation to endometriosis is vitamin D. Some research has suggested that low levels of vitamin D may be associated with an increased risk of endometriosis. Vitamin D is important for bone health and immune function, and it may also have anti-inflammatory effects. However, more research is needed to confirm the relationship between vitamin D and endometriosis.
Another nutrient that has been studied in relation to endometriosis is omega-3 fatty acids. Omega-3 fatty acids found in plant sources, such as flaxseeds and walnuts. Some studies have suggested that high intake of omega-3 fatty acids may be associated with a reduced risk of endometriosis. Omega-3 fatty acids are thought to have anti-inflammatory effects, which may help to reduce the risk of the condition.
There is also some evidence to suggest that low levels of certain minerals, such as magnesium and zinc, may be associated with an increased risk of endometriosis. Magnesium is important for muscle function and bone health, and it may also have anti-inflammatory effects. Zinc is important for immune function and wound healing, and it may also have anti-inflammatory effects. However, more research is needed to confirm the relationship between these minerals and endometriosis. The Flourish ‘Greens’ blend is a good source of magnesium and zinc.
It is important to note that while certain nutrient deficiencies may be associated with an increased risk of endometriosis, it is not clear whether these deficiencies cause the condition. Additionally, the relationship between nutrients and endometriosis is complex and may be influenced by other factors, such as genetics and lifestyle.
What is the research around a plant-based, low fat diet?
There is limited research on the relationship between diet and endometriosis. However, some studies have suggested that certain dietary factors may play a role in the development and progression of the condition. One dietary pattern that has been studied in relation to endometriosis is a low fat plant-based diet.
A low fat plant-based diet is a type of vegetarian diet that is rich in fruits, vegetables, whole grains, legumes, nuts, and seeds, and it is low in fat and animal products. This type of diet is typically high in fiber, antioxidants, and other nutrients that are thought to be beneficial for overall health.
Some studies have suggested that a low fat plant-based diet may be associated with a reduced risk of endometriosis. One study found that women who followed a low fat plant-based diet had a lower risk of the condition compared to women who followed a diet that included more animal products. Another study found that a low fat plant-based diet was associated with a lower risk of endometriosis recurrence after treatment.
There are several potential explanations for the relationship between a low fat plant-based diet and endometriosis. One theory is that a low fat plant-based diet may help to reduce inflammation in the body, which may be beneficial for women with endometriosis. Inflammation is thought to play a role in the development and progression of the condition. A low fat plant-based diet is also typically high in antioxidants, which may help to reduce inflammation and improve overall health.
Another theory is that a low fat plant-based diet may help to regulate the menstrual cycle, which may be beneficial for women with endometriosis. Some research has suggested that a diet that is high in plant-based foods may help to regulate estrogen levels in the body, which may help to reduce the risk of endometriosis.
It is important to note that while a low fat plant-based diet may be associated with a reduced risk of endometriosis, it is not a guaranteed cure for the condition. Additionally, the relationship between diet and endometriosis is complex and may be influenced by other factors, such as genetics and lifestyle..